This judgment was delivered in private. The anonymity of the child and members of the family must be strictly preserved. All persons, including representatives of the media, must ensure that these conditions are strictly complied with. Failure to do so will be a contempt of court
HIS HONOUR JUDGE MARIN :
Introduction
1. J is little boy who is nearly two years old. He has an older brother, H, who is eight years old.
2. Their mother is M. She is 31 years old and has until recently worked in a nursery. Their father is F. He is 40 years old and works as a bus driver. M and F are married and have been together for around fourteen years.
3. In June 2023, J was admitted to hospital with significant injuries some of which were suspected to be non-accidental.
4. Social services at the Royal Borough of Greenwich ("the local authority") became involved. These proceedings were commenced. An interim care order was sought and obtained in June 2023 and the children removed from the parents.
5. The police arrested the parents on suspicion of grievous bodily harm or actual bodily harm. The criminal investigation is ongoing.
Issues to be determined
6. Prior to J's admission to hospital in June 2023, he had also been admitted in April and May 2023.
7. The local authority seeks findings about the cause of injuries observed on J's first admission to hospital on 24 April 2023, on his second admission to hospital on 6 May 2023 and on his third admission to hospital on 5 June. It also alleges that the parents failed to follow medical advice in a timely manner on 3 May and 5 June 2023. The allegations are contained more fully in a Scott Schedule. M and F both deny hurting J in any way or failing to follow medical advice.
8. This judgment is the court's determination of the matters raised by the local authority.
9. The material in this case is extensive and was contained in a number of files. A core bundle contained case management orders, statements, experts reports and various relevant documents. There were also further files containing police documents, medical notes and records, photographs, contact notes and digital forensic analysis documents.
10. I was also provided with police videos and recordings of calls to the emergency services.
11. The parties filed opening and closing written submissions and chronologies.
12. The local authority and the Guardian were each represented by two Counsel. The parents were each represented by Leading and Junior Counsel.
13. I acknowledge the hard work and diligence of all Counsel in this case which was conducted in a collegiate and professional manner such that the parties can be satisfied that they had the best representation possible at the hearing.
14. I am also grateful to the wider legal teams comprising the parties' solicitors and support staff who also deserve praise for ensuring that this case was properly presented. I particularly acknowledge Ms Jachowicz at the local authority who prepared the bundles and ensured that everything was in place for the hearing to proceed smoothly. Given the amount of documentation, this was no easy task.
15. There were some difficulties along the path to this hearing such as obtaining further disclosure from the police and considering a very late request by the medical experts for further medical evidence. However, an adjournment of the hearing was avoided due to the combined efforts of the court and the parties.
Background
16. I turn now to the background facts in this case.
17. The narrative of events is taken from many sources in the papers. Whilst I recognise that some matters are in dispute, the primary aim is to set the scene.
18. I start on 21 April 2023 being a few days before J first attended hospital on 24 April 2023.
19. J visited the GP as he had a cough. The GP's records noted no serious concerns.
20. On 24 April 2023, M said that she woke up H and J around 7am. M went to the kitchen. J was in the landing area leading the to kitchen so M had an unrestricted view of J.
21. J tried to pull himself up on the left corner of the radiator. His legs went "wobbly". He lost his balance and fell onto the side of the radiator, hit the right side of his forehead on the wall and then hit the floor. He ended up lying face down on the floor. After a minute, M observed about twenty seconds of body jerking in all four limbs and J started to cry and scream for around thirty to forty minutes.
22. M called the 999 emergency services. She was concerned as J's head was getting bigger. They said that as J was not vomiting, they could not "red flag" him to send an ambulance but would send a taxicab instead. M then phoned 111 who arranged for someone to call her back. The caller accessed M's phone to see J on video.
23. M then took J to hospital where he was examined.
24. The medical notes recorded that J had been sleeping more than normal; he had vomited his bottle on two occasions that morning. He was noted to have "a large swelling over his forehead which has been spreading over the day, swelling causing some right eye swelling. No injuries elsewhere."
25. A CT scan was reported as showing a "large extracranial scalp contusion of the frontal region mainly on the right side. No intracranial haemorrhage, space occupying lesion or acute focal intracranial legion is shown."
26. The notes recorded J as having sustained an "accidental head injury with a normal CT scan, otherwise well."
27. As time progressed in A & E however, J was sick and it was decided to keep him in overnight for intravenous fluids and observation. The consultant in charge also advised "to check FBC and clotting." There was also concern about the swelling and bruising getting worse and M reporting that J had not had a wet nappy for seven hours.
28. On 26 April whilst still in hospital, J was seen by the ophthalmology team. A junior doctor examined him who discussed the examination with Mr H, a consultant ophthalmologist who reviewed the examination. The note of the examination recorded the following:
"Paeds team noted initial haematoma at the right side of the forehead which tracked down to the eyes yesterday-report white eyes with full ocular motility prior to lid swelling....
Examination: Bilateral lid ecchymosis and swelling...with right eye swollen shut. Able to prise the right lid open slightly-white conjunctiva, fixing and following, no limitation in ocular motility, difficult to examine the lid reflex. LE conjunctiva white, cornea clear on fluorescein staining, full ocular mobility, normal red reflex."
29. During this admission, no safeguarding concerns were raised by the hospital. The hospital recorded the parents as being "very appropriate throughout time in ED."
30. Nonetheless, the local authority maintains that J was deliberately injured on or around 24 April.
31. On 27 April, J fell again. This was recorded in a message sent by the mother where she described J as "went all wobbly and fell, hitting his head again..".
32. M took time off work to look after J. He returned to nursery on 2 May where the mother was also working at that time.
33. On 3 May, M took J to her GP, Dr S. She said that J had gone off his food and had become "fussy" about his milk.
34. I set out the note of the consultation:
"History: seen with mother
discahrged from hospital last week folowing accidental head injury resukting in bruising over eyes and forehead - has follow up arranged with opthalmology in 1 week
at time of discahrge was only making one wet nappy daily but this has not imporved, very poor oral fluid mother reckons 10oz of fluid and one mouthful of solid food
veries between b=layinga nd being irritable drowsy
mild fever
nursery sent home yesterday due to recessions in chest
bowels opening normally
mother concered that has white coating on tobgue that was nto there prior Medication: Nystatin 100,000units/ml oral suspension 1ml To Be Dropped Into The Mouth Four Times A Day. 28 ml
Examination: Tympanic temperature 37.8 degrees C nurofen at 7.00am irritable
old bruising over eyes
rigth eyelid still a bit swollen
throat red and infalmed
white couated tongue
HS 1+2+0
chest rigth sided wheeze, mild subcoastal receesion
abdo SNT
Comment: given very poor urine output, sx of viral LRTI very poor oral fluid intake for immediate paeds A+E review."
35. Dr S said that he told M to go to A & E immediately. He produced a copy of the letter that he gave the mother for the hospital. The letter was also recorded in his notes. It was a standard letter made up from a template used for such letters which allowed him to transpose the consultation notes into a letter.
36. J was prescribed Nystatin which Dr S explained was an anti-fungal medication and not an antibiotic. It was to address J's white tongue. The need to go to hospital arose out of J's poor urine output and oral fluid intake.
37. M understood Dr S to say that J had a throat infection for which he prescribed oral antibiotics. She did not understand him to say that J needed to go to hospital immediately. M also said that she was not given a letter by Dr S. The local authority criticises M for failing to follow Dr S's advice. It also claims that the parents' inaction placed J at risk of harm as the events of 6 May revealed.
38. On 4 May, J appears to have bumped his head in the night. M sent a message to CW where she remarked that the "swelling had come up again" and that she thought that J had bumped his head in the night.
39. On 6 May, J was having blueberry porridge for breakfast. M said that his lips suddenly turned blue and became swollen and his breathing was heavy. The parents took J to hospital leaving H with a friend.
40. The medical notes recorded that J had eaten something which "has caused his lips to swell and start dribbling." It went on the note that:
"..has bronchitis and crackling noisy breathing-last week fell and hit head has severe bruising around eyes."
41. J was admitted to hospital for observation "post anaphylactic reaction." There were also concerns about J being drowsy since his discharge on 26 April and that his haemoglobin level had fallen from 103 to 75 that day.
42. The hospital gave medication to deal with what was a possible allergic or anaphylactic reaction. J also had an increased temperature and signs of a chest infection. Blood tests showed a drop in haemoglobin that necessitated a blood transfusion. The following day, 7 May, J was given a blood transfusion.
43. On 8 May, J was recorded as improving slightly after the blood transfusion. However, he was noted to be refusing feeds "since yesterday" and had vomited after some bottle feeds. He had watery diarrhoea, was pale and had "sluggish bowel sounds."
44. A CT scan reported a "a large galeal haematoma seen on the right side around the front, parietal and temporal regions with preseptal haematoma overlying the right orbit". The neurosurgery team advised that no intervention was required.
45. During his time in hospital, J's blood was checked. A second blood transfusion was considered at one stage. The doctors also noted (as did M) that "swelling and bruising bilaterally and periorbitally" had increased and there was "fluctuant swelling" in both eyes. On 10 May, J's left eye was barely able to open and on 11 May, J was noted to have "difficulty" opening his eyes.
46. On 14 May, J was recorded as looking pale; both ears were described as being "red/purple swollen"; his eye was "opening better."
47. On 17 May, J was finally discharged from hospital. The parents purchased a helmet to protect J although on 23 May, it appears that he hit his head again. On 4 June, M said that the swelling had gone down and J had "pretty much gone bk [sic] to normal ".
48. The local authority maintained that J is likely to have suffered further injuries between leaving hospital on 26 April and being admitted again on 6 May. Moreover, J's poor health indicated that the parents failed J by not taking him to hospital on 3 May as instructed by Dr S.
49. On 5 June, M said that J was asleep in his crib but woke up crying. It was around 7.30am to 8am. The mother was in the shower but got out when she heard J crying.
50. She noticed a small graze and a bruise on J's head. She did not know how this occurred but assumed that he either bumped his head on the musical box in his cot or on the wooden cot itself. F was not at home when this happened. He had gone to a hospital appointment and taken H with him.
51. M took J to hospital. He vomited on the way and was more sleepy although he was responsive.
52. The medical notes recorded the following:
"L parietal - 15x15mm swelling, erythematous
Area of bruising above left eyebrow
5mm cut and bruising below the left eye
Old bruising under right eye and right side of chin
New area of swelling over the right eyebrow, 22mm scratch above right eyebrow, on forehead with an overlying area of erythema
2 small scabs below the lateral aspect of the right eye
Small area of swelling to the right parietal aspect
Both ears swollen and bruised - 5mm cut on the top of the left pinna
2mm cut behind the right ear
Standing with support Grabbing objects - palmar grasp Looking around, PEARLA "
53. The report of a CT scan noted that:
"CT report - No intracranial haemorrhage, space-occupying lesion or acute focal intracranial lesion is shown. No skull fracture is shown. Previously there was a large right frontoparietal extracranial soft tissue contusion/ haematoma as shown on previous CT scans. There is some residual, reduced swelling at this location now."
54. Around 3.30pm, M asked the nursing staff if she could go for a walk with J. They agreed as he had been in the hospital by then for eight hours. M was reported to have been "very compliant and appropriate with [J] and the staff." In fact, M left the hospital.
55. The hospital records note that at 5pm, M telephoned the hospital and spoke to a nurse. The nursing note sets out what transpired:
"Telephone call received in Children's ED from female who introduced herself as [J]'s mother.
She was requesting if I could disclose the findings of [J]'s blood results.
I explained that I am no longer involved in [J]'s care and he has been referred to Paediatrics.
As the intention was to admit [J] she could return to ED and the SpR would happily discuss this with them.
She advised she was unable to do this, I enquired as to why and was advised that she cannot go into detail as the reason she cannot return is personal.
I discussed with SSN Jo Schilling and to her advice is that they should not have left the hospital and the mother had advised she was taking [J] for a walk.
I notified the Paeds SpR immediately as I was aware this case was potentially a safeguarding admission and she made contact with mum."
56. Dr DJ was the Registrar who was dealing with J. The nurse told her about M's telephone call. Dr DJ therefore phoned M and her note sets out what transpired:
"I called Mum back immediately stating that we need to admit [J] so she needs to come back to hospital. I explained that I have spoken to the consultants and we need to admit [J] to further investigate and get to the bottom of what is causing the bruising. We are concerned about the extent of bruising from an insignificant injury. Mum stated she will come back but would not given us a time.
Mum called back about 10-15 mins later asking what would happen if she didn't bring [J] in. I explained that we would have to call the police and inform social services. We are concerned about [J] from a medical point of view and therefore we want him to be admitted. Mum handed the phone to Dad who was very angry. Stated that:
- He does not trust us as the last admission lasted 2 weeks and we didn't find out the cause of the bleeding/bruising
- He feels [J] is fine and there is nothing wrong with him. He was told to look out for boggy swellings which he does not have - Asking how long he will be admitted for. I explained that I don't know how long it will be and it depends on the investigations needed
- Stated that they have an older child and we are splitting up their family. States that the 7yo will become very distressed at not seeing his Mum or brother
- States that he will need to do the school run for his older child which he cannot do. He can't afford to take time off work and won;t be able to pay rent so they won't have anywhere to live.
- Stated that he 'doesn't want to hand his child over to us' and that we are threatening him and leaving him with no choice as we will have to call the police.
I tried to offer solutions including getting family and friends to help with school runs and look after the older child. I have also explained that Mum and Dad can swap on the ward so Mum can go home to spend time with the older child.
Dad very angry despite this. I explained I will again speak to the consultants and call them back but suggested that I don't think the decision re. needing to admit will change."
57. Dr DJ discussed the matter with her consultants who agreed that J needed to return to hospital for what was described as a "safeguarding work up" and that the police should be called if they did not return. She phoned M who agreed to bring J back to the hospital which they did at 7pm.
58. Another doctor saw M and F. The notes recorded the conversation with them:
"Parents and [J] seen by Dr B.... Explained the following:
- We are concerned about the extent of bruising that [J] has
- We have spoken to the haematology team who have explained that all their investigations are normal. There is one test still to be done but this is also expected to be normal
- We therefore need to further investigate and get to the bottom of what has caused the bruising
- We are obliged and legally bound to investigate all children who have unexplained bruising with a skeletal survey - this is multiple x-rays of all the bones to look for any breaks/fractures. Explained to parents that we recognise this is difficult but we are not accusing them of abusing their child. We have to however follow our guidelines and do what is in the best interest of the child.
- We will also get medical photography to take photos
- He will have an ophthalmology review tomorrow
- We will take some photos on the A&E camera now and also do a body map."
59. The next day, 6 June, a consultant spoke to the parents to explain what was happening and also gave them a safeguarding leaflet.
60. J was seen by Mr H, the consultant ophthalmic surgeon. He recorded that there were "multiple bruises at different stages of healing" and that there was a "subconjunctival bleed." He noted that "injuries consistent with N.A.I."
61. Later that day, the police arrived at the hospital and arrested both parents. They were taken to the police station and interviewed under caution. J remained in hospital.
62. J and H were placed under police protection. H was placed with his maternal grandmother. J was discharged from hospital on 8 June and placed in foster care.
63. The local authority claims that J suffered further injury on 5 June and raised concerns about J being taken home from hospital that day and the reluctance of the parents to return him to hospital.
64. Thereafter, proceedings commenced as I have said, an interim care order was made and the children were placed with their maternal aunt where they remain.
The Law
65. I turn now to the relevant law. I set out the main principles although I also have regard to the parties' legal submissions and the various authorities to which they refer.
66. To state the obvious, these proceedings are public law proceedings where the local authority may ultimately seek a care or supervision order. If so, it must pass what is called "the threshold". This is found in section 31(2) of the Children Act 1989, which provides that:
"(2)A court may only make a care or supervision order if it is satisfied:
(a) that the child concerned is suffering or is likely to suffer significant harm; and
(b) that the harm or likelihood of harm is attributable to:
(i) the care given to the child or likely to be given to him if the order were not made, not being what it would be reasonable to expect a parent to give him
The other limb of the test at section (2)(b)(ii) is not relevant in this case.
67. When determining the allegations made by the local authority in the Scott Schedule that comprise the threshold findings, the court needs to have in mind certain matters.
68. The burden of proof in respect of the allegations falls on the local authority who brings these proceedings and who have identified the findings that it asks the court to make.
69. Where a matter has to be proved, the burden of proof is the civil standard, namely the balance of probabilities. To quote Lord Hoffman in Re B (Children) (2008, UKHL 3520):
"...If a legal rule requires a fact to be proved (a "fact in issue"), a judge or jury must decide whether or not it happened. There is no room for a finding that it might have happened. The law operates a binary system in which the only values are 0 and 1. The fact either happened or it did not. If the tribunal is left in doubt, the doubt is resolved by a rule that one party or the other carries the burden of proof. If the party who bears the burden of proof fails to discharge it, a value of 0 is returned and the fact is treated as not having happened. If he does discharge it, a value of 1 is returned and the fact is treated as having happened".
70. There is no obligation on the parents to provide, much less to prove, an alternative explanation for the allegations made (see Lancashire -v- R, W and N [2013] EWHC 3064). The burden of proof cannot be reversed (see Re M (Fact Finding: Burden of Proof [2012] EWCA Civ 1580). The seriousness of the allegation or consequences of fact finding do not affect the need to make findings on the balance of probabilities (see Re BR (Proof of Facts) [2015] EWHC 41).
71. Findings of fact must be based on evidence. As Lord Justice Munby (as he then was) observed in Re A (A Child) (Fact-finding hearing: Speculation) (2011 EWCA Civ 12):
"...It is an elementary proposition that findings of fact must be based on evidence, including inferences that can properly be drawn from the evidence and not on suspicion or speculation."
72. I also have regard to the comments of Dame Elizabeth Butler-Sloss P in Re T (2004) EWCA Civ 558 regarding the need for the court to survey to wide canvass of evidence:
"...Evidence cannot be evaluated and assessed in separate compartments. A judge in these difficult cases must have regard to the relevance of each piece of evidence to other evidence and to exercise an overview of the totality of the evidence in order to come to the conclusion whether the case put forward by the local authority has been made out to the appropriate standard of proof.
73. The evidence of the parents and any other carers is of the utmost importance. It is essential that the court forms a clear assessment of their credibility and reliability. They must have the fullest opportunity to take part in the hearing and the court is likely to place considerable weight on the evidence and the impression it forms of them (see Re W and another (Non-accidental injury) [2003] FCR 346).
74. I direct myself to the fact that the parents may have particular reasons for lying and that those lies do not necessarily mean that their evidence is also untruthful about other matters (R v Lucas, 1981 1 QB 720).
75. I also recognise that human memory is not infallible (see Gestmin -v- Credit Suisse [2015] EWHC 3560). In Lancashire County Council v The Children [2014] EWFC 3 Mr Justice Peter Jackson (as he then was) opined that:
"...I would only add that in cases where repeated accounts are given of events surrounding injury and death, the court must think carefully about the significance or otherwise of any reported discrepancies. They may arise for a number of reasons. One possibility is of course that they are lies designed to hide culpability. Another is that they are lies told for other reasons. Further possibilities include faulty recollection or confusion at times of stress or when the importance of accuracy is not fully appreciated, or there may be inaccuracy or mistake in the record- keeping or recollection of the person hearing and relaying the account. The possible effects of delay and repeated questioning upon memory should also be considered, as should the effect on one person of hearing accounts given by others. As memory fades, a desire to iron out wrinkles may not be unnatural – a process that might inelegantly be described as "story-creep" may occur without any necessary inference of bad faith."
76. Medical evidence must be considered in the context of all the evidence.
77. In A County Council v K D & L [2005] EWHC 144 (Fam) Mr Justice Charles observed that:
" 39. To my mind it is important to remember:
i) that the roles of the court and the expert are distinct, and
that it is the court that is in the position to weigh the expert evidence against its findings on the other evidence, and thus for example descriptions of the presentation of a child in the hours or days leading up to his or her collapse, and accounts of events given by carers. ...
44. ....in cases concerning alleged non accidental injury to children properly reasoned expert medical evidence carries considerable weight, but in assessing and applying it the judge must always remember that he or she is the person who makes the final decision."
78. This view was endorsed by Mr Justice Baker (as he then was) in Re JS (A minor) [2012] EWHC 1370.
79. When assessing expert evidence, I also have in mind that cases involving a multi- disciplinary analysis of the medical information conducted by a group of specialists, each bringing their own expertise to bear on the problem, the court must be careful to ensure that each expert keeps within the bounds of their own expertise and defers, where appropriate, to the expertise of others (see Re S [2009] EWHC 2115 (Fam)).
80. When seeking to identify the perpetrators of non-accidental injuries, the test of whether a particular person is in the pool of possible perpetrators is whether there is a likelihood or a real possibility that he or she was the perpetrator (see North Yorkshire County Council v SA [2003] 2 FLR 849.
81. In Re S-B (Children) [2009] UKSC 17, Lady Hale SCJ held that:
"....if the judge cannot identify a perpetrator or perpetrators, it is still important to identify the pool of possible perpetrators. Sometimes this will be necessary in order to fulfil the "attributability" criterion."
82. I turn now to the evidence.
The Medical Evidence
83. The medical evidence comprised doctors who gave expert opinions in this matter and doctors who were involved in J's care last year.
84. The expert medical evidence developed as the case progressed. It is thus found in reports prepared by the experts, correspondence dealing with questions raised and a transcript of a meeting between all of the experts.
85. At the experts meeting, the view was taken that a report from a consultant geneticist was advisable. This was obtained in time for the experts to consider it before the hearing. Crucially, it allowed the experts to finalise their view.
86. The experts are all respected specialist doctors whose reports were well written and helpful. Rather than simply repeat the contents of their reports, I shall summarise some key points that emerged from their evidence. That a particular matter or fact is not contained in my summary does not mean that I have ignored it or that it has a lesser importance.
87. By way of introduction, it is helpful to clarify some medical terms used by the experts which featured heavily in the case.
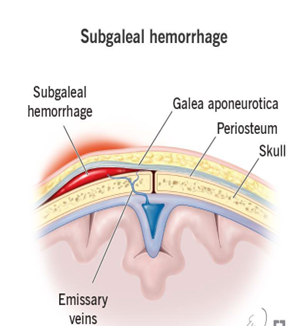
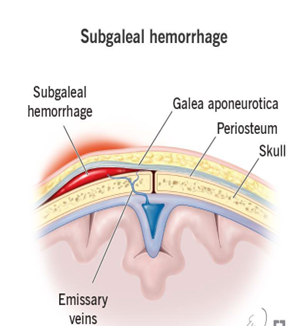
88. Subgaleal refers to the location of the condition which is on the head between the skin on the scalp and the skull; or in medical terms between the periosteum and galea aponeurotica.
89. A haemorrhage designates that there is active or ongoing bleeding in the subgaleal area of the head. It is usually observed in neonates after delivery by vacuum assistance and in children with minimal head trauma, such as hair combing or braiding.
90. A hematoma identifies bleeding that clots, which changes from a liquid to a partially solid form caused by rupture of the emissary veins.
91. I have included a diagram of the head in the Schedule to this judgment to put the area under discussion in context. The diagram did not form part of the evidence but was one that I utilised for my own assistance.
92. A subconjunctival haemorrhage is when a blood vessel breaks in the white of the eye. Blood builds up below the conjunctiva and causes a flat, bright red patch in the white of the eye. It is similar to a bruise on the skin.
93. Mr Jayamohan is a consultant paediatric neurosurgeon. He gave oral evidence at the hearing.
94. The following emerged from his evidence:
(a) One possibility for J's injuries could be a head injury inflicted on J when he was hit multiple times over a period of months.
(b) Another possibility was that there was an impact such as the one described by M in April that was followed by evolution of injuries caused by the redistribution of bleeding from the subgaleal haematoma.
(c) Subgaleal haematoma's were:
"...rare in toddlers but are seen with neonates who usually have difficult deliveries and these are often associated with instrumentation. So, the level of force required does seem to be usually significant (as is involved during instrumentational deliveries) and involving some level of trauma."
(d) Whatever the court's findings about the cause of the injury, it was still unusual because of its progressions over the months. J's case should be considered on an individualised basis.
(e) J's presentation was unusual and also an unusual way to sustain a subgaleal haematoma. However, it was a possible mechanism. In these rare cases, statistical analysis did not help.
(f) A subgaleal haematoma should resolve after two months to the point that it was as if J had not had a "subgaleal space injury." This also meant that during the two month period, J was vulnerable to reinjury. Thus, following the April incident or an accidental fall, the tissue remained vulnerable to reinjury from normal handling or force that was not the result of an abusive act.
(g) When asked about the physical and physiological processes likely to have been at play when J sustained his subgaleal haematoma, Mr Jayamohan referred to a shearing or sliding mechanism which caused movement of the scalp in relation to the underlying bone and tissue so as to rupture the vessels bridging the space; a sliding motion rather than a straight impact. Although an unusual fall, if the head moved against a hard surface in a downward or scraping/shearing motion, the vessels could bleed which would lead to the subgaleal haematoma.
(h) Reinjury could not take place by the further significant force being inflicted but by the application of a lower force; this would include those seen in a domestic environment. However, the presentation would appear to be abusive.
(i) It was "in the parent's favour" that there were photographs and clinical notes of the scalp changes whilst J was in hospital. Without this information, Mr Jayamohan said:
"I would be less pushing of my suggestion that this may be an exuberant reaction, he shows a rapid change even in the first couple of days and the medical records which document change almost under the eye of the paediatricians."
(j) An impact between the head and the side of the cot or on the music box in the cot could account for the June injuries.
(k) There was no significance to the fact that prior to 24 April, when J had fallen or bumped himself, he did not react the same way.
(l) If there had been significant intracranial injury to the brain, Mr Jayamohan said that he "would not be voting for the radiator incident as a potential cause of the injury."
(m) When asked about a scenario where the injury had not happened as described and it would mean that J had suffered inflicted injuries on several occasions, Mr J answered that:
"If I am incorrect with my possible hypotheses this boy has been hit multiple times over a period of months but I don't see any evidence of brain disfunction clinically and there is nothing on the brain scan, he would have to be hit enough to cause the scalp injury but not enough to cause anything else, it becomes equally unlikely doesn't it?"
95. Mr Jayamohan's comments about the injuries made at the expert's meeting are important to note:
"So there is clearly a swelling that was just right sided that would fit with an impact, but which had then significantly increased to be all over the forehead and around by the time he was in hospital. So unless we're going to opine that after the 999 call, this child had another head injury, so with no reported one, it would have to be a further inflicted head injury after the 999 call and video check had been done, there seems, from the clinical evidence of a right sided forehead bruise, followed by an egg sized bruise, followed by across the whole forehead bruise, progression from that one area of impact over that time period. So that was my logic for saying, "Yes, this is really rare, but it's also really rare to get a child who's got multiple or very significant swellings from impacts. Let's suggest then, if it was multiple, it would be an inflicted injury, but without any intracranial injuries whatsoever.
So either of these options is unusual, but I couldn't really see a way that I would say that the non-accidental multiple impacts without brain injury are a higher likelihood than the single impact and then the exuberant or the unusual subgaleal swelling. Is that a fair summary, Ms Allan and chaps, of what I said and I shared the screen? If you want, I can do that again to just explain it, but it's a subgaleal haemorrhage that was seen in this case, so I'm not saying that there isn't, hasn't... there couldn't be multiple non-accidental impacts to this child's head. I guess what I'm saying is that would be quite unusual without any brain injury, albeit within the limits of CT scan. Now, the other way, the scalp swelling would be unusual, but they both kind of seem as 2 possibilities, which eventually I think is not down to us to make that call."
96. Dr Keenan is a consultant paediatric haematologist who carried out extensive tests on J's blood. He was not called to give evidence as his unchallenged conclusion was that "the bruising and bleeding observed in [J] should be considered to have occurred in a child with a normal blood clotting system".
97. Dr Cardwell is a consultant paediatrician. He gave oral evidence. His view was that:
(a) Subgaleal haematomas are "uncommon in children" and were "more reported in the neonatal period with an association with ventouse delivery...which can result in shearing of the emissary walls."
(b) He deferred to Mr Jayamohan regarding the development and evolution of the subgaleal haematoma.
(c) A subgaleal haemorrhage is associated with "a shearing force that disrupts the layers of the scalp."
(d) Some of J's injuries could be non-accidental and some accidental.
(e) If M's account of the 24 April was accepted, it could explain the injuries to J that day.
(f) The injuries in June could have resulted from the fall described by M which would be secondary to the underlying abnormality of the scalp from April and the tissue on the head and face being vulnerable to injury at a lower force.
(g) The injuries in June could also be the result of inflicted injury as a result of blunt trauma.
(h) The magnitude of the forces applied to the head in May and June were not significant and would not normally give rise to the injuries seen on
(i) The evolution of the injury after April made the tissue on the head and face vulnerable to further injury from a reduced level of force.
(j) The subconjunctival haemorrhage was unlikely to be as a result of blood tracking from the subgaleal haematoma.
(k) On 5 June, J appeared to have suffered new injuries of a linear abrasion and subconjunctival haemorrhage which could have been caused by a new injury or trauma.
(l) J may not have come to harm as a result of not going to hospital on 3 May and instead going on 6 May.
(m) He deferred to Dr Lavy regarding the cause of the subconjunctival haemorrhage.
98. Dr Lavy is a consultant ophthalmic surgeon. He gave oral evidence and the following emerged:
(a) He accepted the opinion of Mr Jayamohan and the possibility of the evolution of the injuries, even though it was rare. This theory was also valid for the whole presentation of J's head including the periorbital region.
(b) The subconjunctival haemorrhage seen in J's right eye on 6 June could have appeared after the injuries that occurred on 24 April.
(c) The subconjunctival haemorrhage could have resulted from the April injury.
(d) An intervening injury was a possible cause of the subconjunctival haematoma. It was also possible that it existed since April.
(e) The nursing notes on 24 April and 7 May recorded J reacting to light. Commenting on the suggestion that these examinations were not consistent with the suggestion that the subconjunctival haematoma could not be seen in April due to swelling, Dr L said that it was because one did not have to open the eye that much to see the cornea and pupil. To exclude a subconjunctival haematoma, the eye would have to be opened considerably more to be sure that one was not present. Moreover, the nurses were doing neurological observations to check that the pupils were equal and reactive to light and they would not be looking for a subconjunctival haematoma
(f) The subconjunctival haemorrhage was not observed in May as the examination was conducted by a nurse whose examination would not necessarily reveal its existence.
(g) The existence of a subconjunctival haemorrhage was not necessarily the result of an inflicted injury.
(h) There was only one subconjunctival haemorrhage and because of the way these develop, it was difficult to make too much of this in terms of an indicator of non-accidental injury.
(i) There was no separate ophthalmic or periorbital injury sustained before the May admission.
(j) The injuries seen on 5 May and 6 June are likely to be the same injuries resolving and the photographs do not demonstrate that there were fresh injuries in May.
(k) The subconjunctival haematoma could manifest itself in the same way over time as the main injury did.
(l) The April injury was hard to attribute to falling against a radiator and onto the floor.
(m) Regarding the mechanism for the subconjunctival haematoma:
"[J]developed very marked black eyes around both eyes and both eyes closed over. That says to me there was further spreading of blood or bleeding in or around the eyes. It is not inconceivable to me that the bleeding could have been deeper. The black eyes are because of bleeding in the lids, and subconjunctival haematomas are essentially from in the tissues around the eye so a subconjunctival haematoma could appear subsequent to the first injury in the same way as the black eyes developed subsequent to the injury."
(n) He also stated that:
"The conjunctiva is the skin on the surface of the eye so either trauma to the surface such as a snag from a fingernail or it comes from further back behind the eye, and comes up underneath the conjunctiva. Anatomically, a classic black eye is caused by blood in the eye socket which is similar in origin to a subconjunctival haematoma coming from behind or around the eye, and being seen underneath the conjunctiva. And therefore in the context of a child with so much bruising around the eyes, a little bit of extra blood under the conjunctiva would not be enough to suggest another cause for the subconjunctival haematoma. I would put that together with the massive bruising around the eye and say that whatever caused the bigger injury caused the subconjunctival haematoma. Not that I am right but there is not any reason to think two different injuries here."
99. Dr Irving specialises in clinical genetics. She prepared a report. Her conclusions were accepted and she therefore did not give oral evidence.
100. Dr Irving did not identify any factors that would raise a concern about an underlying genetic disorder; there was no underlying genetic cause as the reason for J's presentation to hospital with extensive bruising in May 2023; J did not have Ehlers- Danlos Syndrome ("EDS") or any other genetic disorder; there was no other condition that would make him susceptible to bruising.
101. Three doctors who treated J at some point were called to give evidence. I have already referred to their involvement in the background narrative.
102. Mr H, the consultant ophthalmic surgeon, saw J on 26 April and on 6 June.
103. He accepted that he was not an expert in the field of bruising following a subgaleal haemorrhage. He said that a subconjunctival haemorrhage could occur accidentally. He recorded J's injuries in June as non-accidental because of the bruising.
104. Mr H had little recollection of how J appeared when he saw him on 26 April. He accepted that a junior doctor examined J and discussed the matter with him.
105. Dr DJ saw J on 24 April in A & E. On that occasion, she reviewed him and after discussion with the consultant, he was admitted to hospital.
106. She also saw J on 5 June. I have already referred to her notes which set out what transpired.
107. Dr DJ recalled the parents returning to the hospital at 7pm on 5 June. She did not recall that F was aggressive or angry when he returned to the hospital and if he had been, it would have been written in the notes. Equally, she did not recall F apologising for his behaviour earlier that day.
108. J's GP, Dr S, said that his notes were written during the patient consultation. The notes said that he told M to take J to hospital because of his poor urine output and reduced oral intake. He was sure that he would have printed off the letter for the hospital in accordance with his normal practice. He would also have emphasised that M should go immediately to hospital as he recorded in the notes.
Conclusions of the Expert Medical Evidence
109. I am very grateful to the medical experts who spent much time not only preparing their reports but considering matters further as more information became available. I also want to acknowledge Dr Irving who came late to the case and was still able to produce a detailed report very quickly.
110. The doctors who gave evidence were all specialists in their fields and gave helpful and focussed answers. They all explained matters carefully and with thought. I am grateful for their input into this case.
111. Whilst in no way diminishing the standing and evidence of the other medical experts, Mr Jayamohan deserves particular recognition. He was very impressive. Mr Jayamohan was a key expert in this case and embraced that role. His answers to questions were razor sharp and clear leaving no room for doubt. I found him to be the most helpful medical witness.
112. Turning to the lay medical evidence, Dr DJ recalled J and gave helpful evidence. Dr S came across as a competent and diligent doctor. I found Mr H to be somewhat vague and his evidence was not particularly helpful. Albeit completely understandable, he did not come across as really recalling J in much detail.
113. The following emerged in my judgment from the expert medical evidence.
114. First, it was clear that J's condition was unusual and should be considered on its own merits.
115. Second, there were two possibilities to explain J's injuries.
116. The first is that they were caused with an impact on 24 April followed by an evolution of injuries caused by the redistribution of bleeding from the subgaleal haematoma.
117. The second is that J was hit multiple times over a period of months. Dr Cardwell raised the possibility of a third option being a hybrid causation with some injuries being accidental, others non-accidental which I also accept.
118. Third, it was also open to the court on the medical evidence to decide whether the injuries evidenced an accidental or non-accidental injury or a hybrid. In either situation, a low impact force will have caused the injuries given the absence of brain injury or skull fracture.
119. Fourth, ultimately what transpired is a matter for the court and in that regard, the parents' evidence was crucial to form an understanding of events.
120. Fifth, much was said about the subconjunctival haemorrhage.
121. It was seen on 6 June both on examination and in pictures. The question arises whether it was present earlier.
122. Against it being present before 6 June is the fact that it was not seen on examination on 26 April or 7 May. Instead, Mr H and medical staff at different times recorded that the eye was clear or at least that no subconjunctival haemorrhage was observed.
123. In favour of the subconjunctival haemorrhage being present before 6 June is that first, Dr Lavy explained how the examinations carried out by nurses might not have picked up the subconjunctival haemorrhage. Second, Mr H did not examine J on 26 April; a junior doctor carried out the examination and then discussed the matter with Mr H so it could have been missed. Third, the possibility existed that the subconjunctival haemorrhage manifested itself the same way as the subgaleal haemorrhage and thus appeared later.
124. It seems to me though that the answer is really found in the picture evidence. A picture of J on 6 June clearly showed J with the subconjunctival haemorrhage. A clear picture on 19 May did not reveal anything. By May, the effect of the subgaleal haemorrhage was observed; if the eye was to follow the same course, the subconjunctival haemorrhage should also have been present by that time. It was not, however. It seems more likely than not taking everything together that the subconjunctival haemorrhage was not present in April and May but was a new event first observed in June.
The Lay Witness Evidence
125. Turning to the lay witness evidence, Ms DG worked in the same nursery as M.
126. She had known M for under a year as a co-worker. DG described M as kind and caring. There were no concerns about the way M worked at the nursery. M always engaged with the children and ensured their needs were met. DG also said that J was well looked after and that he had a good relationship with M.
127. DG described how she visited M in hospital and that M was upset and worried about J. DG was shocked when the children were removed from their parents.
128. Ms JW was the manager of the nursery where M worked. They had worked together for three years in a professional capacity.
129. She described M as "brilliant" with the children and said that M had asked to do extra training.
130. Although the baby room at the nursery could be hectic, when M was there it was calm. M took everything in her stride. She would sit and sing to a crying baby. J was also at the nursery and JW M as being "wonderful" with him and them having an "amazing bond."
131. JW visited M when she was in hospital with J. She described M looking as if she had not slept and with worry over her face.
132. JW was "completely and utterly shocked" and not able to "get my head around it" that the police and social services were involved with the family.
133. Ms LB is J's maternal grandmother. She was clearly distressed when she gave evidence about the events of the last year and very nervous. She did her best nonetheless to help the court.
134. LB said that M had always wanted to work with children from a young age. M loved her job at the nursery and was a good mother. She also explained that before J was born, M would go to her home when she had an argument with F "rather then screaming or shouting" in front of H.
135. DG, JW and LB did their best to assist the court. I gained little from LB's evidence which seemed to be somewhat confused at times. DG and JW's evidence was helpful as it spoke about M generally and her work with children and her relationship with J.
The evidence of the parents
136. M and F both gave evidence over the course of a day. They were extensively cross- examined. They were both asked several times whether they had lied to the court, the police and/or social services and whether they had caused injury to J. M and F were adamant that they were telling the truth and had not caused any injury to J.
137. Prior to this matter, there had been no adverse findings against them by social services although they were known to them.
138. H made allegations in 2020 about being pinched and there was bruising on his arm in 2021 caused when playfighting with M. That year, H also said that M squeezed his hand tight and made him sometimes sleep on the floor.
139. In 2022, H's school referred regular bruising and scabs on H to social services.
140. On every occasion, investigations were undertaken which revealed no issues of concern with the parents albeit that advice about safe play was given in 2022.
141. Both parents filed statements and answered questions put to them to the best of their ability. The parents' evidence though revealed a number of deficits both as to their relationship and regarding the events between April and June 2023.
142. F told the police that his relationship with the M was "perfect." However, he did not really explain this in the context of messages where he berated M for not making his sandwiches and calling her lazy.
143. Although F said he was not present on 24 April or 5 June when the injuries were said to have occurred, F was adamant that he believed M to the point that he had not even read her witness statements. He had also never discussed the events of April to June with M.
144. I found this hard to accept between parents who must have been concerned about what was going on in their lives. It also did not fit with a message sent by M on 5 June to a relative saying that F was blaming her for everything and that he would "never forgive me if J gets taken into care."
145. F accepted being angry on the telephone to the hospital on 5 June. F clearly did not want J at hospital that day. It was clear that he placed pressure on M to leave and to not return to the hospital. This left M having to tell the nurse on the phone that she could not return for personal reasons.
146. When matters reached the point where it must have been obvious to F that they had to return to the hospital, F was rude on the telephone. F said that he apologised for his behaviour when he arrived at the hospital. Dr DJ though had no recollection of any apology nor was one recorded in the hospital notes.
147. M referred to F being a frustrated person and LB recounted to the police that M would take H overnight to her house to avoid the screaming and shouting at home although she said in her oral evidence that this had occurred only once. F accepted that if he had a bad day at work M "got the brunt of it" although he denied that he was a generally aggressive or angry person.
148. In her interview with the police though, when M was asked about the events leading to J's return to hospital on 5 June, she was also asked about the F. She referred to him shouting, being controlling, sometimes angry and rude.
149. I reproduce the relevant extract from the interview as it is instructive both in terms of the events on 5 June generally but also in respect of the picture painted by M of F:
"DC H: Okay. At this point were police mentioned at all by the hospital?
M: Only when I called them and asked about the bloods and then my husband took the phone off of me and started talking to them.
DC H: Okay, so yeah, that was around 5pm, hospital sort of flagged up that you didn't return and a call was made, you said to the hospital staff on the phone, 'What will happen if [J] was not brought in?' Why did you ask that?
M: 'Cause my husband was asking me.
DC H: Okay.
M: And I asked them to repeat it when they were on speaker.
DC H: Okay and was your husband listening to the conversation telling you what to say?
M: He took the phone.
DC H: Okay. And you said, you've said, sort of said to me that you were worried, you wanted his injuries checked, why would you leave and go home?
M: Because he told me to.
DC H: Okay, are you scared of your husband?
M: I'm not scared of him, he's just a little bit controlling.
DC H: A bit controlling, okay. Okay. Right, and in that sort of phone conversation, take your time by the way, if you do need a minute. And in your own words [J]'s dad took the phone, how would you describe his sort of mood when he took that phone call?
M: Angry.
DC H: Okay. So I'm aware on the phone call that [J]'s dad said that [J] is fine, he was also complaining about the rent being paid and getting time off work, didn't want to bring [J] in and he said that the hospital were threatening with police getting involved. How do you feel about sort of [J]'s dad sort of prioritising that over [J]'s wellbeing?
M: I don't think it's acceptable, you know, it should have been his son, and be like, 'No, you need to stay there'.
DC H: Okay, so would you describe him as being quite an angry person?
M: Sometimes.
DC H: Okay. And how often would you say he gets angry?
M: It depends what the situation is.
DC H: Okay, and does he get angry towards you?
M: He shouts at me and, he's never hit me or anything like that, he just shouts and raises his voice, stuff like that sort of thing.
DC H: And you mentioned he's quite controlling, sort of describe to me what you mean by controlling?
M: Like if I go out, 'cause I don't go out very often, if I do I always take the kids with me, he gets the hump if I go out or like last, when was it, Saturday he told me I don't do nothing and that I'm lazy and stuff like that.
DC H: Okay, so [J] was brought back to the hospital around 7pm with you and your husband. The hospital described you as being completely silent, almost numb and that [J]'s dad sort of took over and was quite irate, quite angry, in their own words they have described him as angry.
M: Yeah.
DC H: How was you feeling at that moment?
M: Just upset that I left.
DC H: Okay, and when you say he told you to come back, how did he say it? Can you kind of remember what the conversation was?
M: Angrily on the phone, it was like, 'If you, you need to be in a taxi, I want a text to say that you're on your way back, if you're not then I'm coming up there and kicking off'.
DC H: Okay, and why do you think he, that was his reaction?
M: Probably because I didn't call him to say that [J]'s hurt himself. "
150. Examination of F's phone revealed deleted messages from E, a female work colleague.
151. Starting at 4.16am on 31 May 2023, E messaged:
"My kind of attitude, I am not gud at making revenge
but I can ignore ur existence like I never meet u in my life...
...Pple need to learn that their actions do affect other
pple...so be careful what u say and do ..."
152. Another message on 31 May at 3.25pm stated:
"Why is it that no matter how much pain it endures by holding on...the heart refuses to let go?
...Dnt ever make someone Ur everything...cos if U loose
them U will have nothing...."
153. At 4.05am on 2 June:
"Happy birthday to a smart, kind and truly gorgeous
soul. Blow out those candles and take the next year
by storm. Sto latek!!!..."
154. At 2206 hrs the same day:
"Had a lovely evening..thank U soo much I really
needed after stressful day.."
155. The local authority suggested that these messages indicated that the F was having a relationship with E.
156. F denied any relationship with E. They were work colleagues. Messages were sent early in the morning as E and F were on duty. F deleted not only E's messages but also other messages. F described how he was "OCD ish" about messages only retaining those from significant people such as M.
6 This extract is taken from the interview transcript; only the officer's name and the mother's name have been altered.
157. On behalf of F, it was said that the messages from E could be read many ways. The reference to the night out and having a good time referred to an occasion when a group of work colleagues went out together. There was a message from another (male) colleague which also appeared to refer to the same event.
158. To my mind, these messages do not necessarily evidence a relationship between F and E. The reference to "be careful what u say and do" could also have so many meanings.
159. However, in the context of events that were going on at that time in the life of the family, I found it difficult to understand how F could justify going out regularly with work colleagues when M was left at home and there was nothing to suggest she had any real social life. The so-called group outing was at the end of May, a short time after J had been admitted on two occasions to hospital between 24 and 26 April and 6 and 17 May.
160. Indeed, M told the police on 6 June that she did not go out very often and when she did, F "gets the hump." F going out was even more striking against the background of his job, its unsocial hours and the concomitant effect on the family and especially M of his absence.
161. The parents had been together for fourteen years. My overall view is that the relationship was not at all perfect. F could be rude and angry and felt able to place pressure on M to the point that she told the police that she felt controlled. F felt able to go out with work colleagues at a difficult time for the family. M did not seem to have much of a life outside the family home. F felt able to blame M when things went wrong and get upset if M went out. Added to all this was the concern about money which F mentioned as a concern if M was in hospital with J and unable to work. F was to later increase the pressure by his behaviour on 5 June and his overriding concern that an admission to hospital would split up the family.
162. None of this painted a "perfect" relationship. If anything, it appeared a rather one-sided relationship that was not happy or smooth.
163. I turn now to the specific events between April and June so far as the parents' evidence raised concern.
164. For his part, F maintained that he was not present on 24 April and 5 June but as I have said, he accepted M's account of events.
165. M's evidence was as unsatisfactory as it was worrying.
166. I would have expected M to set out her account of events that transpired in those few fraught weeks last year with some fluency obviously allowing for nerves whilst giving evidence. Instead, she delivered an account that was inconsistent and at times made no sense.
167. I start with the events of 24 April.
168. In her first witness statement, she said J fell on the radiator valve. In her second statement filed a day before the final hearing and in cross-examination, she said he fell on the side of the radiator.
169. M also said that J hit his head on the wall as he fell down and there were "multiple impacts". When describing the event in evidence though, she referred to a sliding motion down the wall after the radiator. This had never been mentioned before.
170. She told the ambulance crew that J did not cry but told the emergency services handler that he did cry. H saw everything that happened but to the police, M said that he was in the shower.
171. In her latest statement, she said that J had started to pull himself up during the Easter weekend on 7 to 10 April; in her first statement and in her police interview, it was the weekend of the 22 and 23 April.
172. M said that F turned on the radiator when he got up around 3am to 4am and then she turned if off at 4.30am to 5am. That made no sense at all. By 7am when she got up, the house would be cold again and there was no reason why a radiator would be turned on for such a short period of time when its effect would be minimal. This also raised the question of whether the radiator was hot when J fell against it and if it was, why M left him near that area or did not remove him quickly when he started to topple.
173. Of even more concern is that the picture of J's injuries on 24 April does not fit with M's description of what happened. It shows two vertical grazes present on the head. That does not fit with falling onto a radiator nor sliding down a radiator and/or a wall.
174. What is really worrying is that having gone over the M's account in its various forms, considered the picture evidence and the layout of the house, I really struggle to understand what exactly happened on 24 April. M's account simply made no sense. I am somewhat fortified in this concern because the experts too had trouble trying to understand the mechanics of the fall.
175. If J wobbled and fell onto the radiator, how did he end up also sliding down the wall? Would he not have fallen backwards on downwards on the radiator? How did he get from the radiator to the wall? Why did M not grab him when she saw the fall start? If the radiator was hot, that certainly made sense aside from the question of what he was doing there in the first place.
176. Regarding the visit to Dr S on 3 May, M said that Dr S gave J antibiotics and she decided to wait and see how he managed before going to hospital. The medication that Dr S prescribed was in fact antifungal medication for J's tongue.
177. M denied receiving any letter from Dr S to give to the hospital and did not understand Dr S to instruct her to take J immediately to hospital.
178. Dr S said he was concerned about J's poor fluid intake and urine output which formed his decision that J should go to hospital "immediately," which is what he noted in his contemporaneous record of the consultation.
179. I accept Dr S's evidence that the record was contemporaneous as he typed whilst dealing with the patient. This is also apparent from the spelling errors in the record. The record would therefore contain the words used by him to M.
180. The record also referred to a letter which Dr S said was composed from a standard template on the record system. Dr S was adamant to the point of saying he was ninety- five percent certain that he gave M the letter and told her to go immediately to A & E. That was his normal practice.
181. Dr S came across as a competent and diligent doctor who was very sure of his practice. I accept that he gave M a letter to take to hospital in accordance with his normal practice. The letter was included in the consultation record. There was nothing about sending the letter another day or sending it direct to the hospital.
182. Indeed, any child with J's immediate medical history of having recently been discharged from hospital and presenting the way he did at the surgery on 3 May would clearly need attention.
183. I really fail to understand how M could have misunderstood such that she decided to wait and see how J's health progressed, that she believed that his medication was an antibiotic and that also believed that she did not need to go to hospital immediately. But this is what she messaged to others; M, a person well educated and practised in childcare.
184. On 4 May, J bumped his head. By this time, there can be no doubt that J was unwell. He had seen the doctor the previous day. According to M, he was on antibiotics as he was "poorly" but she did not take him to hospital nor did she proffer any explanation. She even said in cross-examination that she had no regrets about waiting until 6 May to take J to hospital.
185. When describing the events of 5 June, M said in her statement that J was asleep in his cot and she was in the shower. That is also what she told Dr DJ. However, when interviewed by the police her story changed to say that J was awake:
" ..J was still asleep but he started to stir so I put him into his cot, so at that time was having a cuddle, he fell back asleep, the he started to stir so I put him back into the cot and I was getting into the shower.."
186. M also sent a message to F that morning saying that she "thought he would be ok in his cot for a couple of minutes" which suggested that J was awake.
187. Of course, if J was awake, he was not wearing his helmet or some other head protection which by then M and F had felt he should wear.
188. M was asked about the cot and how J could have been injured. When interviewed by the police at the hospital, the body worn footage revealed M to say that J only had a teddy bear and a blanket in the cot. She repeated that to Dr DJ at the hospital that day. However, when interviewed by the police on 6 June, M said there was a teddy bear, blanket and a music box.
189. The music box was not in earlier photographs produced but was in the photograph taken by the police at the time of the June incident.
190. M said that the music box was purchased to soothe J after the May admission. The music box was a hard object. In the context of parents purchasing a helmet for J and being concerned for the safety of his head, it made no sense to put a hard object such as a music box in J's cot. Indeed, the medical evidence is that the music box could have caused injury to J. Moreover, a picture of the cot on 19 May did not reveal a music box although I accept that it could have been purchased later.
191. The local authority referred me to pictures of the cot taken in June by the police. A baby bag, bottles and keys were lying in the cot.
192. It was suggested that this was an attempt by M after she left hospital to set a scene to support J's injuries. I do not accept that theory. None of these items in the cot could have caused the injuries sustained by J. M said that she threw them in the cot when she went to hospital.
193. Whilst I approach M's account with caution, I cannot draw anything from the state of the cot and cannot conclude that the music box suddenly appeared on 5 or 6 June.
194. The events later that day when M left the hospital are of concern.
195. M asked the nursing staff if she could go for a walk with J as she had been at the hospital for many hours and the nurse agreed.
196. Instead, M went home without telling anyone. M said that she thought it was alright to go home. That made no sense because no one had told her it was permissible and safe to leave. Moreover, she sent a message to F saying "walked out on way out" to which F replied "what did they say" to which M replied "Advised me not to go." Despite this message, F felt able to say in cross-examination that he knew of no reason why M could not leave the hospital.
197. M had no right to take J home from hospital. She did so without permission and in circumstances where J had suffered further injuries which the hospital needed to investigate. Her actions put J at risk and neglected his health needs.
198. I am also clear that M did not want to return to the hospital. She only returned around two hours after her conversation with the hospital and in circumstances where Dr DJ told her that if she did not return, the police would be notified. This left M with no choice but to return.
199. I am also satisfied that M was under pressure from F to return home and stay there. F claimed to be worried about the family being split and the financial considerations of M not working if J were admitted to hospital.
200. F had no right to be angry with the hospital. All they were doing was their job which was to care for J and understand what had happened to him. Moreover, F should have put J before his concerns about money and splitting the family. Whilst I accept that parents faced with a sick child can react in different ways, F's reaction was not acceptable. He placed pressure on M to return home, to stay at home and when that seemed unlikely, he vented his anger on the hospital. He said that he apologised but as I have said, it was never recorded, and I do not believe him.
201. Were the injuries caused deliberately?At this point, I stand back and consider the whole of the evidence. I give no special status to the expert evidence and carefully weigh everything I know about the parents.
202. I also have in mind the observations of Sir Mark Hedley in London Borough of Southwark v A Family [2020] EWHC 3117 (Fam), when he said:
"182. If ever there was a case in which the court had to retain the big picture, both for the controversial and the uncontroversial evidence, this was it. Much of my time over the last four weeks in preparing this judgment has been spent not in writing or organising but in careful reflection on that big picture. In the end, I have come to a conclusion that the Local Authority has failed to prove its case to the requisite standard. In reaching that position, I also have to recognise that I have no clear answer to give as to how S died, since, and this is really common ground, none of the canvassed alternative suggestions could be clearly established....
187. Since this is at least the second time that I have concluded after a long forensic enquiry that I do not know what has happened, I need to ask myself one hard question: is this simply a failure of judicial nerve to make a finding against a family such as this, the finding which is nevertheless required by the evidence as a whole? I ask that question not just because it occurred to me but also because I recognise that decisions in cases like this are not driven exclusively by the process of reasoning.
188. There is an element in human judgment that lies beyond cold rationality as every experienced trial judge soon comes to appreciate. In order to test that, I have reflected carefully upon the position as it would be were I to have found that the Local Authority had indeed established their case and this child had been sexually assaulted and killed by one or more members of a family who had then conspired to conceal the truth from all legitimate enquiry. I discovered that such a conclusion would be an affront to my judicial conscience."
203. I refer to my conclusions about the medical evidence. I have spent considerable time going over not only the extensive papers in this case but the evidence as a whole and more particularly, the parents' evidence. I have arrived at my decision after giving consideration and anxious thought to this matter.
204. Sadly, I have concluded that J's injuries were deliberately inflicted. I do not believe that the parents have given truthful evidence to the court.
205. I have carefully considered reasons why M and F might have not told the truth.
206. M may have wanted to avoid an acceptance that her relationship with F and her life generally was not perfect.
207. She lived with a man who could be controlling; that was certainly evidenced in the events of 5 June and how M left the hospital in accordance with F's instructions.
208. M may have been stressed by arguments which at least on one occasion led to her removing herself from the family home to stay with LB. M also seems to have had a lonely life.
209. For his part, F seemed to place the maintenance of the family unit and the family income as a high priority especially as the events of 5 June demonstrated. It may be that F believed that everything needed to be done to preserve the family unit.
210. F's need to cover the realisation that his relationship with M was a long way from the "perfect" that he described to the police may also have contributed to not telling the truth. This might explain why he was adamant that he never questioned M's version of events which some may feel any normal person would do in the circumstances F found himself in with J coming to harm when he was not at home.
211. Nevertheless, do these potential reasons or explanations allow the court to conclude that the core of the parents' evidence was nonetheless truthful? In my judgment, they do not.
212. I have taken into account that M is dyslexic and how that might affect the inconsistencies in her evidence, as well as the possibility of story creep. I also note that the hospital initially had no concerns about the parents who presented as caring and loving parents.
213. The various messages at times provide a prima facie contemporaneous narrative of what was happening or going through M's mind as well as evidencing concern of both parents about J. Indeed, throughout the forensic analysis of the parents' electronic devices, there was seemingly no message that revealed anything sinister or untoward.
214. M also spoke quickly to the emergency services on 24 April and did not object to them having a video call to observe J. M and F took steps to protect J by fitting a radiator guard and buying a helmet and when F was arrested, he held J carefully when taking him back to the ward.
215. I also have in mind that the medical evidence supported a view that the injuries could be the result of an accident and were evolving which was observed under the eyes of the doctors in hospital when there was no opportunity for J to be harmed by his parents and that the presentation of J on 6 May was entirely consistent with an allergic reaction. There is also the fact that M took J to hospital on 5 June.
216. These are all points which cannot be dismissed, and which could go towards an outcome in favour of the parents' case that J was not deliberately harmed by them or anyone else.
217. Standing back though and looking at the wider canvass, there are other matters of serious concern which cannot be ignored, and which place the so-called positive points in perspective to the point that in my judgment, they heavily weigh the scale against the parents.
218. When considering the injuries, it is necessary to consider them in the wider chronology of events. Accordingly, I shall include in my discussion other events upon which the local authority also seeks findings.
219. I have set out my view of the parents' relationship. F's picture of a perfect relationship was untrue. F was a man who felt able to pressurise M not to leave the hospital and to try and make her remain at home on 5 June. This was controlling as I have said. F was an angry person at times; certainly not afraid to shout at M or the hospital. He also felt able to go out with work colleagues when M seemed to just stay at home.
220. Despite F being a person who felt able to tell M freely what to do and do as he liked, it made no sense that he never discussed the events surrounding J's injuries with M and he never questioned M about what happened. This seemed the obvious thing for any couple to do especially when F said that he was not present in April or June.
221. Indeed, this certainly did not sit well with M's message saying that F blamed her for everything and F's fear of the children being taken away and the family being split to the point that he was prepared to allow J to forgo hospital investigations and possible treatment.
222. There are also the incidents in April and June where I feel unable to simply ascribe the contradictions and deficits in M's evidence as being down to story creep, nerves when giving evidence or dyslexia. Her evidence revealed serious deficits which cannot be ignored.
223. I would have expected a normal parent to recount consistently and clearly albeit with the odd embellishment or error, the events surrounding J's injuries. M did not. As I have explained, her account of key events was often contradictory. The story about how J fell on the radiator on 24 April made no sense. The photographic evidence of J did not fit her description of what happened on any basis. That M contacted the emergency services soon after the alleged fall on the radiator cannot remove M's failure to provide a proper account or an account that properly explains what happened.
224. On 27 April, J fell again. M described this in a message as J "went all wobbly, and fell, hitting his head again." To the police, she said that he fell against soft furnishing which she described as pillows and toys. M and F did nothing about this incident.
225. Whilst the fall may have been harmless in normal circumstances, J had been discharged from hospital the previous day; his head had been hurt and he had suffered injuries which were getting worse at that time. In those circumstances, the very least M and F could have done was to contact the GP or dial 111 to seek advice. Instead, they did nothing.
226. Talking about the event in messages somewhat aggravates the fact that they did nothing because they clearly saw it as an event that was worthy of comment but equally did not see the need to seek some professional reassurance not to worry or to ask whether they needed to do something.
227. Then there are the events of 3 May. This evidenced a complete failure to act appropriately in J's best interests.
228. J had been discharged from hospital a week earlier. The GP's notes recorded a child who was clearly not doing well at all; poor oral fluid intake, only one wet nappy daily, one mouthful of solid food, drowsy and irritable.
229. In these circumstances, any parent would not have been surprised to be told that the child needed to be seen at hospital. J was obviously unwell. Nonetheless, M seemingly misunderstood the doctor's instruction to go immediately to A & E, she denied receiving a letter for the hospital and thought J had been given antibiotics. This was an experienced mother with an older child and who was qualified in childcare being the profession she had always wanted to follow and study. I have already said that I accept Dr S's account and prefer his evidence to that of M.
230. Frankly, a child presenting as J did that day and given his recent discharge from hospital did not require a GP to say that J needed medical help. It should have been obvious. Indeed it was; the problem was that M did not want to hear or take that course of action. She did not want to go to the hospital.
231. I accept that Dr Cardwell felt that J may not have come to harm by not going to hospital on 3 May. However, that does not preclude a finding as to how the court believes M should have acted in the circumstances and in the face of Dr S's advice. I also cannot overlook the fact that J required a blood transfusion when he was admitted and how he was generally unwell. His condition may not have medically been different on 6 May to his medical presentation on 3 May but from a welfare perspective, there was a failure to act responsibly and in J's welfare interests.
232. There is one apparent oddity in all of this though. M messaged others that day to say that she had antibiotics for J and was keeping an eye on him. I do not accept that M was foolish enough or lacked the intelligence to understand or be able to follow Dr S's instructions. M either deluded herself or deliberately sent out a smokescreen to others. I cannot believe that she genuinely held this belief.
233. The events of 5 June also raise serious questions about the parents.
234. M's evidence left the court with no clear picture of what happened on 5 June.
235. It was unclear if J was asleep or awake and whether M went into the shower knowing that J was awake without his helmet or not. There can be no basis for M's unclear account. A genuine parent would know such basic details of whether their child was awake or not and recount exactly what happened. Once again, there is no issue of "story creep" or other factors.
236. Turning to events at the hospital, every parent knows that sitting and waiting in A & E is time consuming and worrying. Long periods of time can elapse before much happens or between seeing one doctor or having some test or x-ray.
237. However, a committed parent also knows that their child's health and welfare demand that they remain in hospital until the medical staff tell them that they may leave.
238. M told the staff that she wanted to go for a walk. In the circumstances of A & E, this was not an improper request and the nursing staff agreed. Instead, M took J home and did not intend to return. It was only when she tried to obtain J's blood test results that the hospital realised that she was not there and that she should not have gone home.
239. At the point when M was told that test results could not be given over the phone, she should have returned to hospital. She said there was personal reasons for not returning. This was F who was telling her not to return and who was obviously wound up and frustrated about the need to return. In the event, it took Dr DJ to effectively demand that she return under the threat of social services and the police being involved. That still did not stop F from taking the phone and shouting at Dr DJ in protest about returning.
240. None of these events on 5 June were the actions of committed and caring parents. Once again, J's welfare interests were second to the wishes of M and/or F in not wanting to return.
241. The reason for not returning was the alleged fear of admission to hospital and the concomitant loss of income and the family being broken up with H having to stay elsewhere. I accept that these matters would weigh heavily on a parent although in the circumstances of this family, they had to be secondary to J's needs.
242. However, in the context of J who had by this time been admitted on two occasions and who was unwell generally, M and F's behaviour and reactions were utterly wrong. They were entitled to worry about their financial and family issues but they should have realised from the start that J needed medical care. Instead, they failed him by trying to avoid that care.
243. J's medical presentation situation was unusual as I have said. Indeed, so unusual that it led the medical experts to offer alternative opinions and state that J's situation needed to be considered in its own right. Crucially, none of the medical experts ruled out non- accidental injury caused by one or multiple impacts albeit by a lower level of trauma.
244. Thus, the medical evidence allows for a finding that someone deliberately injured J. The only possible perpetrators were M and F.
245. The deficits in the parents' evidence are many and serious for the reasons I have given. The failure to seek medical help on 27 April and 3 May was wrong and a failure to act properly. The events of 5 June regarding the hospital were unacceptable. I also refer to my findings about the parents' relationship.
246. What emerges is that I find myself completely unable to accept M's account of what caused J's injuries. Instead, I was left with accounts that are so questionable that I simply do not believe what I was told. The overall picture of events in those few weeks between 24 April and 5 June is so worrying. Everything leads me to conclude that J was injured on more than one occasion. He did not have any accident or accidents. The only matter I do accept is that in May, he had an allergic reaction to his porridge but that changes nothing.
247. I also refer to my finding about the subconjunctival haemorrhage which was seen in June for the first time. It is more likely than not that this was the result of a further injury that was inflicted.
Who caused the injuries?
248. The next question is who caused the injuries.
249. On 24 April, F was at work. M sent him pictures. Pictures taken prior to 24 April show that J was well and unharmed. Reference was made to a message sent on 22 April by F to his sister saying that he was "having a mare" looking after the children together with evidence that F was "terrified" generally of looking after J does not in my view take matters further.
250. M and F said the photo on 22 April was taken in the evening although there was a suggestion that it was taken that morning and the injury could have been inflicted later that day. However, that is questionable when considering the messages on 24 April between the parents, M sending F a picture and the emergency services and the hospital not questioning that the injuries could have been earlier than that morning. It is more likely than not that the injuries were inflicted on the morning of 24 April. I find that only M could have inflicted the injuries on J that day.
251. On 5 June, F was not at home as he had a hospital appointment. Again, the messages between F and M support the fact that F was not present when J came to harm and that J was hurt at a time when F was not at home. I find that only M could have inflicted injury that day.
252. I also find that injuries could well have been inflicted on other occasions.
253. I have referred to F being angry. However, on the balance of probabilities, I am unable to make a finding on the evidence that F caused injury to J. However, I do find that F was aware at some point of the truth of what happened. It is more likely than not that his behaviour on 5 June was borne out of a concern that the truth of the situation would emerge especially when messages revealed that he was quick to blame M and concerned that the children would be taken into care which was of itself a strange reaction.
254. I am clear though that it is more likely than not that M caused the injuries. I cannot though explain what caused M to act as she did. Given the positive aspects that I attribute to her, this needs careful exploration.
255. Regarding the findings sought by the local authority about both parents' failure to follow medical advice, I have already set out my view which is that on 3 May, M failed to follow the advice of Dr S. F was not at the consultation. I make no finding against F because there is the possibility that he relied on what M told him. In respect of the events of 5 June though, both parents failed J. Leaving hospital and the reluctance to return J was unacceptable and a serious abrogation of their role as parents in the circumstances.
256. I reject the suggest that the events of 3 May and 5 June were makeweight allegations that do not deserve a threshold finding.
257. Given my findings, the threshold for the making of public law orders is passed.
258. That is my judgment.
SCHEDULE